
As the world of healthcare grows increasingly complex and disjointed, V12 Network stands out as a proven solution. With over a decade of research and development, our flagship provider network management application serves some of the nation’s largest payers and providers. Built on Salesforce, V12 Network delivers a powerful provider data model paired with practical, real-world workflow automation across the entire provider lifecycle continuum.
V12 Network – The Ultimate Provider Network Management Solution
Health Insurance/Payers
Direct to Employer Health Plans
Health Systems
Managed Care Organizations
Integrated Physician Networks
Post-Acute Care Organizations
Value-Based Care Networks
Specialty Network Providers
Third Party Administrators
Say goodbye to complexity with V12 Network. Our platform facilitates seamless collaboration between providers and payers, eliminating fragmented information and disjointed workflows. Consolidate all provider-specific processes into a single platform, establishing a single source of truth for your organization.
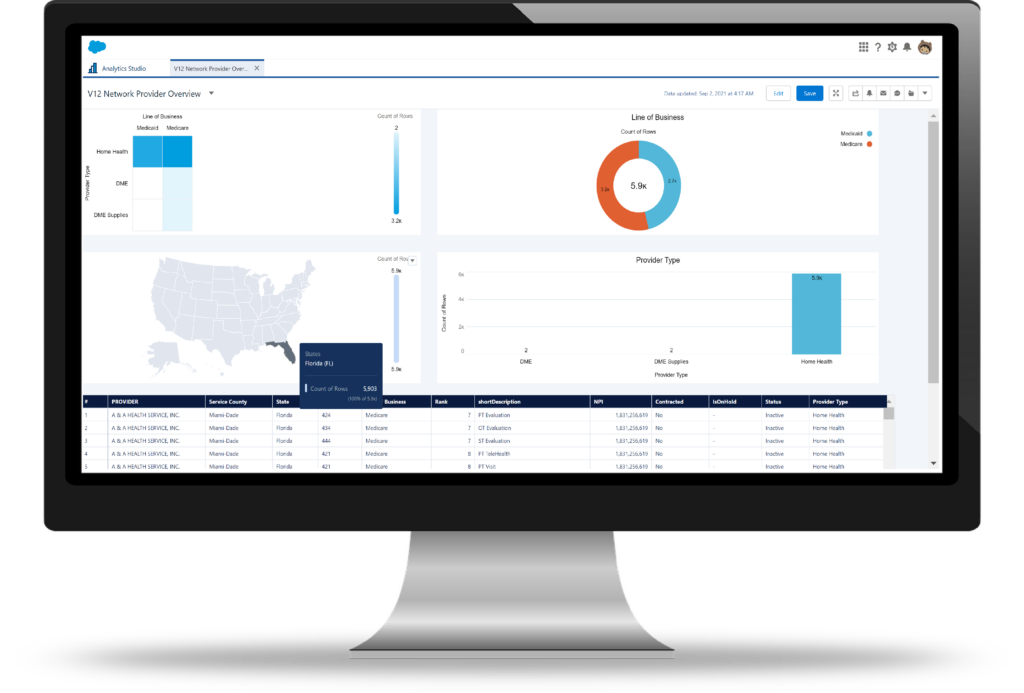
V12 Network is meticulously crafted to address the distinct needs of healthcare organizations. From initial outreach and network development to credentialing, contract management, and post-claims workflows, we provide a 360-degree view of both provider data and crucial workflows.
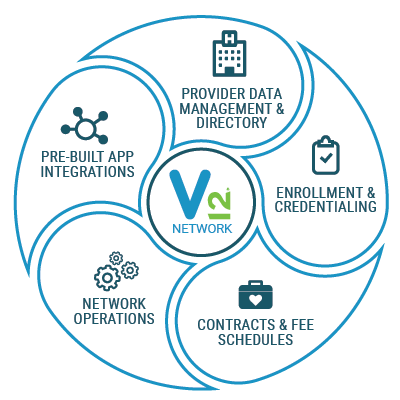
Streamline your provider data management and maintain an accurate directory.
Simplify the enrollment and credentialing process for providers, ensuring compliance and efficiency.
Manage contracts and fee schedules effortlessly, ensuring transparency and accuracy in billing.
Optimize network operations with real-time insights and analytics, enabling proactive decision-making.
Seamlessly integrate with pre-built applications to extend the functionality of V12 Network and enhance user experience.
Reduction to Produce the Provider Directory
Reduction in Time for Provider Directory Updates
Reduction Time in Lead Set Up
Reduction Time In Account Set Up
Reduction Time in Multiple Location Entry
Days Saved Annually for Data Transfer
Implement Results in as Quickly as 90 Days
Lower Administrative Costs
Deprecate Existing Antiquated Technology
Increase Interdepartmental Collaboration
Decrease Provider Onboarding Time
Streamline Tedious Network Operations Workflows
Increase Provider Directory Accuracy and Directory Compliance
Elevate Real-Time Analytic Reporting
Increase Provider Satisfaction Scoring (CSAT/NPS)
Increase Provider Directory Accuracy
You asked, we listened! V12 Network is now compatible with Salesforce Sales Cloud, Service Cloud, and Health Cloud. At Virsys12 we are focused on meeting you wherever you are at in your implementation journey.
Ready to learn more about our different product offerings? The breadth and functionality of V12 Network spans far beyond one page of information, but this quick, in-depth overview will help you start digging in.


Whether you have a few quick questions, want a full demo of V12 Network or find yourself somewhere in between, we’re here to help.
Can’t wait? Call us at (615) 800-6768.
"*" indicates required fields
Virsys12
278 Franklin Road, Suite 300
Four CityPark
Brentwood, TN 37027
solutions@virsys12.com