Your onboarding process sets the tone for your entire network development journey. Get it right, and you’ll earn praise from your teams for seamless experience continuity. Providers may even start to see healthcare as less fractured than before. But if you miss the mark, brace yourself for negative feedback on provider CSAT/NPS scores and potential financial setbacks due to delayed claims and billing activation.
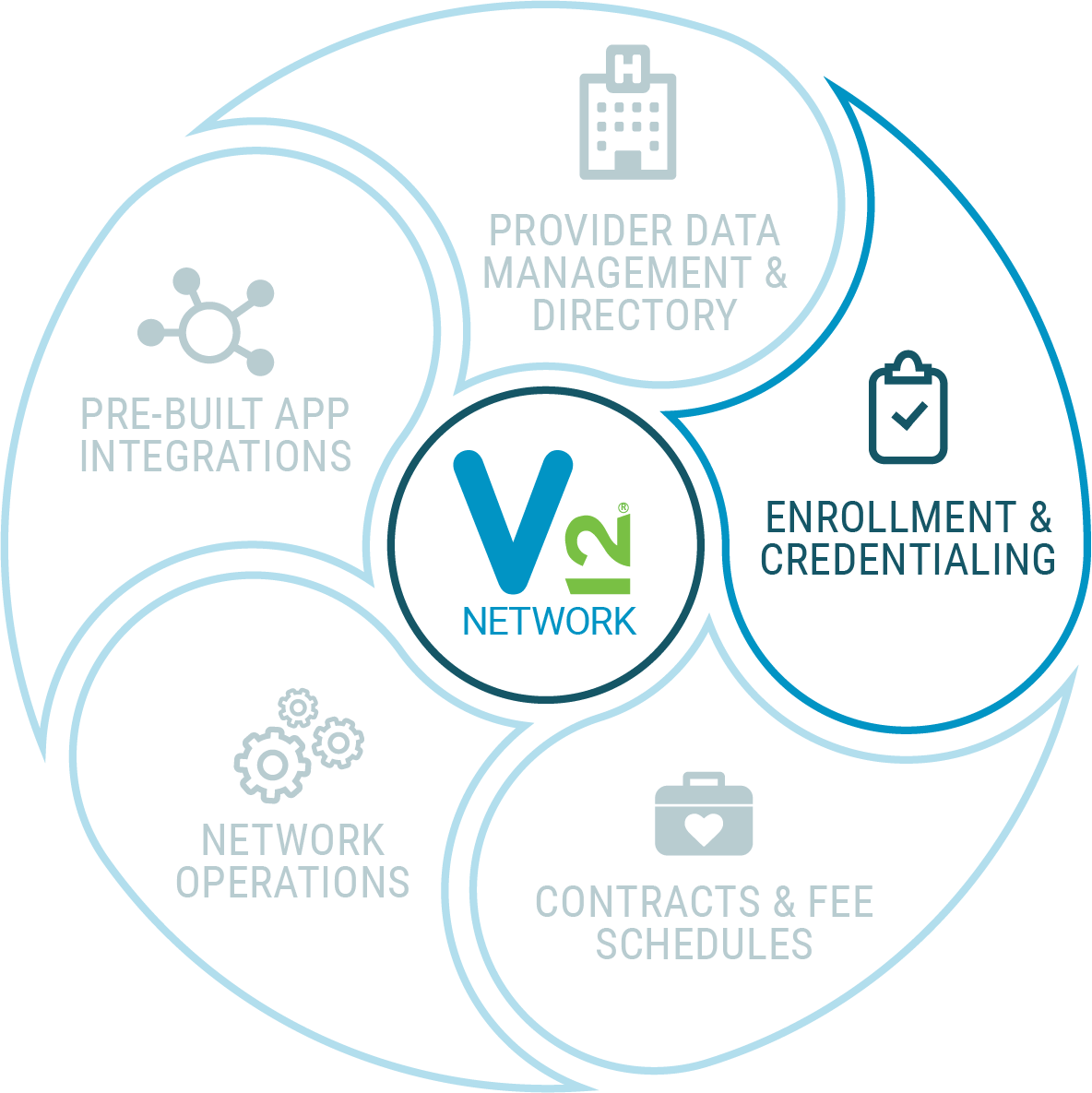
The V12 Network application offers pre-built enrollment and credentialing workflow automation designed for various business models. Whether you’re a health plan or other organization embarking on network development while navigating state-specific enrollment and credentialing guidelines, or a provider operating in a delegated model, we’ve got you covered.
Don’t let a cumbersome enrollment process hinder your success. Streamline with V12 Network today.
Robust Provider network application and form management capabilities
Pre-built integration capabilities with CAQH Provider Data Portal to pre-populate provider attested data within V12 Network
Support of multiple credentialing models such as inhouse, CVO, and delegated entities
Itemized storage of critical credentialing data such as Licenses, Accreditations, Certifications, Privileges, etc.
Ingest Provider roster files and automatically create credentialing cases for seamless workflow transition
Pre-built business rules to prompt key credentialing steps such as primary source verification and exclusion/sanction management with optional CVO integration
Manage Re-credentialing and provider attestment workflows post initial cred process
Trying to understand and manage the complex many-to-many relationships involved in provider network management starts with the provider application process.
Provider and payer organizations are continually challenged to collaborate and complete the necessary applications and steps required in a way that is efficient and scalable. Allowing your prospective and active providers to apply for a network online is quick and easy with V12 Network.
Credentialing is the pivotal step in the provider network process and can be the most complicated and tedious process in the entire provider lifecycle. But it doesn’t have to be that way. Whether your organization performs in-house, delegated works with a CVO, the credentialing process with collaboration and automatic OIG check are a readily available for your team. V12 Network has you covered!
Once you receive the provider information, it has to be validated for accuracy before initiating the credentialing process. What if you could check the practitioners OIG and state exclusions real-time and follow an auditable and structured workflow process to stay on track?
You can with the automation in V12 network with API integration to industry leading CVOs for exclusion checks!
Whether you have a few quick questions, want a full demo of V12 Network or find yourself somewhere in between, we’re here to help.
Can’t wait? Call us at (615) 800-6768.
"*" indicates required fields
Virsys12
278 Franklin Road, Suite 300
Four CityPark
Brentwood, TN 37027
solutions@virsys12.com